Human antibody response to vaccination
Understanding the human antibody response to vaccination
Antibodies are one of the most remarkable features of the adaptive immune system, and their striking properties have contributed greatly to the success of vaccination strategies. Several diseases remain, however, for which immunisation regimens are unable to induce a highly effective and long-lived antibody response. In recent years we have established protocols for detailed studies of the humoral immune response to different types of vaccine, using a combination of systems serology, immune repertoire and serum analysis. In addition, we have been able to identify and characterise panels of monoclonal antibodies (mAbs) from vaccinated volunteers. This work allows us to deepen our understanding of the humoral response to different antigens and vaccine formulations and informs the design of next-generation vaccines that induce stronger antibody responses, as well as potentially leading to the development of prophylactic and/or therapeutic antibodies.
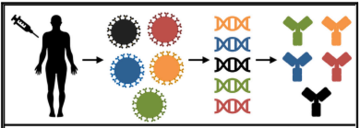
From vaccinated volunteers to mAbs
We isolate mAbs from vaccinated volunteers using an in-house single B cell sorting and variable region cloning platform that allows us to efficiently isolate and express new recombinant mAbs. These are then characterised using a variety of assays, including functional neutralisation activity assays, as well as structural studies to map neutralising epitopes on the antigens. The structural work is undertaken in close collaboration with our neighbouring research group led by Prof Matt Higgins.
Understanding the human antibody response to PfRH5 vaccination
The RH5 protein from the deadly P. falciparum is essential for red blood cell (RBC) invasion during malaria infection. Blocking the interaction between RH5 and its RBC receptor basigin can supress RBC invasion, thereby preventing further growth of the parasite. Importantly, RBC invasion is extremely rapid, requiring less than 30 seconds to complete. Thus, to be successful, a vaccine needs to induce very high levels of potent antibodies against RH5 that act rapidly against this moving target. Using functional and structural studies of antibodies targeting RH5, we have been able to map the key epitopes in RH5 that are targets of the most potent neutralising mAbs. In addition, we have identified a class of antibodies that do not directly inhibit parasite invasion, but that has the ability to slow it down, affording additional precious time to block RBC invasion by the neutralising antibodies. This type of discovery is then fed back into our subunit vaccine design process, allowing us to develop “immuno-focussed” vaccination strategies that have the potential to induce more potent responses by enriching the response with these more effective antibodies.
For more information:
Alanine, Daniel GW, et al. "Human antibodies that slow erythrocyte invasion potentiate malaria-neutralizing antibodies." Cell 178.1 (2019): 216-228.
Payne, Ruth O., et al. "Human vaccination against RH5 induces neutralizing antimalarial antibodies that inhibit RH5 invasion complex interactions." JCI insight 2.21 (2017).
Wright, Katherine E., et al. "Structure of malaria invasion protein RH5 with erythrocyte basigin and blocking antibodies." Nature 515.7527 (2014): 427-430.
Human antibodies targeting P. vivax
To replicate, P. vivax must invade immature red blood cells through a process requiring interaction of the P. vivax Duffy binding protein (PvDBP) with its human receptor, the Duffy antigen receptor for chemokines. Naturally-acquired antibodies that inhibit this interaction associate with clinical immunity, making PvDBP a leading candidate for inclusion in a vaccine to prevent malaria due to P. vivax. We isolated a panel of monoclonal antibodies from human volunteers immunized in the world’s first clinical vaccine trial of PvDBP and we screened their ability to prevent PvDBP from binding to the Duffy antigen receptor for chemokines, and their capacity to block red blood cell invasion. This identified a broadly neutralizing human monoclonal antibody that inhibited invasion of all tested strains of P. vivax. In collaboration with the Higgins group, we determined the structure of a complex of this antibody bound to PvDBP, indicating the molecular basis for inhibition. These findings will guide future vaccine design strategies and open up possibilities for testing the prophylactic use of such an antibody.
For more information:
Rawlinson, Thomas A., et al. "Structural basis for inhibition of Plasmodium vivax invasion by a broadly neutralizing vaccine-induced human antibody." Nature microbiology 4.9 (2019): 1497-1507.
Payne, Ruth O., et al. "Human vaccination against Plasmodium vivax Duffy-binding protein induces strain-transcending antibodies." JCI insight 2.12 (2017).
Antibodies against Ebola virus
A collaboration with Prof Alain Townsend in Oxford led to the isolation of more than 80 mAbs from volunteers vaccinated with recombinant adenovirus expressing Ebola virus glycoprotein (EBOV GP) and boosted with a modified vaccinia virus Ankara. The antibody response was diverse both in gene usage and epitope recognition, and almost half of the isolated mAbs neutralised GP pseudotyped influenza virus. A cocktail of the most promising antibodies, showing high affinity and targeting non-overlapping epitopes, completely protected in a preclinical model of EBOV infection, highlighting the importance of vaccinated volunteers as a powerful source of potential therapeutic antibodies.
For more information:
Rijal, Pramila, et al. "Therapeutic monoclonal antibodies for Ebola virus infection derived from vaccinated humans." Cell reports 27.1 (2019): 172-186.


